Beyond LDL: The Role of Lp(a) in Cardiovascular Risk.
Understanding Lipoprotein(a): A Critical Cardiovascular Risk Factor
Lipoprotein(a), commonly referred to as Lp(a), has garnered much attention over the last few years, and for good reason. It continues to be one of the most common inherited accelerants in the development of cardiovascular disease, yet it is rarely screened for. If you have done blood work with us, you know what your Lp(a) level is. If you are reading this and you haven't had it checked, then now is the time.
What is Lp(a)?
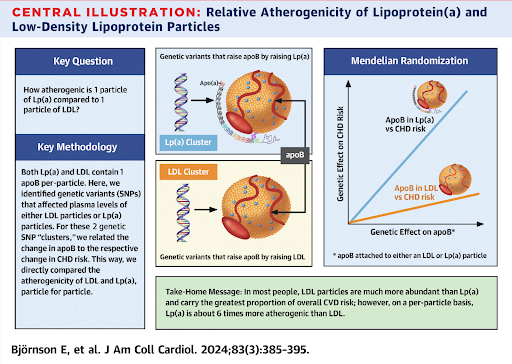
Lp(a) is a low-density lipoprotein that carries cholesterol as well as an apolipoprotein B (ApoB) molecule. It can represent up to 30% of the LDL-C level that you see when you get it tested. What makes Lp(a) unique, however, is not just its pro-plaque characteristics (atherogenic), but also that it is pro-inflammatory and pro-clot (prothrombotic). This is the reason for its disproportionately negative impact. Some studies have indicated that it can be up to 6 times as atherogenic as LDL-C alone (9).
If you have talked with us in the past about cardiovascular disease, we have unpacked how your overall risk depends on much more than your lipid levels alone. Inflammation and endothelial function can be just as important. This is what can make Lp(a) particularly problematic, as it can negatively impact all three of these pathways that elevate your risk for heart disease.
How Lp(a) Damages Your Arteries
Some of the most interesting research on how Lp(a) does its damage is around how it impacts the health of your arteries directly. We discuss endothelial function as one of the main influences on cardiovascular health. We want your artery walls to be supple and resilient. Anything that makes our arteries more stiff and inflamed (see cigarettes) is bad news.
Nitric oxide (NO) is a key molecule made at the level of the endothelium and allows our arteries to dilate and relax. A recent study published this year found that Lp(a) directly inhibits the enzyme that makes NO at the level of the blood vessel wall and increases other free radicals that damage tissue (5). Now we see not only the lipid burden, but increased inflammation and worsening endothelial function all in one particle. Literally a 1-2-3 punch!
Vitamin C and Lysine: A Promising Combination
Now here is where it gets interesting. Vitamin C as a therapeutic agent has been shown to improve endothelial function, and it may have to do with its possible relationship with Lp(a).
Now time for a tangent. Over 20 years ago when I was a medical student, I volunteered at the Haight Ashbury Free Clinic. While there, the president and CEO at the time, Dr. Inaba, told a story about Linus Pauling and his passion for vitamin C. He believed it could play a role in supporting the detox programs in the clinic and was administering high doses of it to patients. The director went on to say how they had to stop the program as the large piles of powdered vitamin C were triggering cravings for other similar appearing white substances. For history on the clinic and its mission, you can read here.
Now where was I? Oh yes! Research from Pauling and others has shown that vitamin C can improve the health of the lining of arteries (10, 6). This likely has to do with how it may counter the negative impact of Lp(a) decreasing NO, as well as serving as an antioxidant to the higher levels of superoxide (free radical) created when Lp(a) is high.
In addition, combining vitamin C with amino acid lysine supplementation seems to mitigate the impact of high Lp(a) even more by making it harder for Lp(a) to grab onto developing clots, thus making your blood less sticky.
Other considerations could be low-dose aspirin or even nattokinase, but these carry other risks and should be discussed with your physician before initiating.
Lp(a) in Women and Menopause
In women, Lp(a) levels appear to increase after menopause and current guidelines recommend that women have levels checked at least once before menopause and then 5 or so years after to verify no significant increase in levels and therefore risk. Another win for hormone replacement therapy (HRT), as it is the drop in estrogen that appears to be related to the rise seen after menopause.
Understanding Lp(a) Levels and Risk
Lp(a) can be reported in both mg/dL and nmol/L, so it is important to know what units the lab is using when reporting your number. Here's a simple guide to understanding risk levels:
Low risk: < 30 mg/dL (roughly < 75 nmol/L)
Intermediate ("gray zone"): 30–49 mg/dL (roughly 75–124 nmol/L)
High / risk-enhancing: ≥ 50 mg/dL (roughly ≥ 125 nmol/L)
Risk for CVD appears to be 1.2 to 3 times higher in individuals with high levels of Lp(a). And this is not just for heart attacks. Valvular disease, peripheral vascular disease, and heart failure risk are all elevated as well.
The Evolutionary Paradox
As with many things in our biology, what was once an advantage has now become a risk (see APOE and parasitic environments). When the risks from uncontrolled bleeding were high (during childbirth, trauma etc.), having molecules that supported the clotting cascade accelerated healing and saved lives. Today, the beneficial aspects are outweighed by the chronic pro-inflammatory and prothrombotic features and increased heart disease risk over a much longer lifespan.
What to Do If Your Lp(a) Is Elevated
If your Lp(a) is elevated, the first step is to assess your other risk factors that we can more easily control. Optimizing blood pressure, inflammation, and lipid markers may be key to slowing progression. In addition, there are other things you can do to lower the negative impacts from increased inflammation, clotting, and endothelial dysfunction.
Current Treatment Options
Niacin: Niacin can lower Lp(a) levels up to 25%, but because it did not show a statistically significant decrease in mortality in large clinical trials, it is not widely recommended by guidelines. Until other therapies are available, if niacin is well tolerated, it is part of the potential arsenal to lower levels. Many people experience flushing from niacin however so it is often a non-starter.
Novel Therapies on the Horizon
There are no fewer than 5 novel therapies in clinical trials to lower Lp(a). Interestingly, studies have shown that those with the lowest levels of Lp(a) can have a higher rate of diabetes (up to 38%). This will need to be watched closely, as drugs have shown the ability to lower Lp(a) levels up to 98%. Will we see a similar uptick in insulin resistance akin to statins? Only time will tell.
Important Note About Statins
It is important to recognize that statin therapy, the traditional first-line pharmacologic intervention for elevated cholesterol, can have varying effects on Lp(a), often leading to increase in levels. Studies have shown this can be up to 24% in some people. This is one reason why PCSK-9 inhibitors may be preferred when LP(a) is elevated, as they have been shown to lower LP(a) up to 30% Remember, cardiovascular disease is multifactorial and the benefits may still outweigh the risks, but this is why assessing each risk category is so important.
Key Takeaways
Lp(a) is a genetically determined, independent risk factor for cardiovascular disease
It causes damage through multiple mechanisms: lipid burden, inflammation, and impaired endothelial function
Vitamin C and lysine supplementation may help mitigate some of the negative effects of elevated Lp(a), although hard outcome data is lacking
Screening is important, especially for those with family history of heart disease or women approaching menopause
While treatment options are currently limited, several promising therapies are in development
Managing other cardiovascular risk factors is crucial when Lp(a) is elevated
References
An Update on Lipoprotein(a): The Latest on Testing, Treatment, and Guideline Recommendations. American College of Cardiology, 2023. https://www.acc.org/Latest-in-Cardiology/Articles/2023/09/19/10/54/An-Update-on-Lipoprotein-a
Nordestgaard BG, et al. Lipoprotein(a) and cardiovascular disease. The Lancet, Volume 404, Issue 10459, 1255-1264.
Kostner KM, Kostner GM. Lp(a) and the Risk for Cardiovascular Disease: Focus on the Lp(a) Paradox in Diabetes Mellitus. Int. J. Mol. Sci. 2022, 23, 3584. https://doi.org/10.3390/ijms23073584
Tsimikas S, Gordts PLSM, Nora C, Yeang C, Witztum JL. Statin therapy increases lipoprotein(a) levels. Eur Heart J. 2020 Jun 21;41(24):2275-2284. doi: 10.1093/eurheartj/ehz310. PMID: 31111151.
Zubiran R, Remaley AT. Lipoprotein(a) and the Vascular Redox Interface: Linking Arteriosclerosis, Thrombosis, and Vascular Biology. Arteriosclerosis, Thrombosis, and Vascular Biology, 46, 1, (248-250), (2025). https://www.ahajournals.org/doi/10.1161/ATVBAHA.125.323880
Rath M, Pauling L. Hypothesis: Lipoprotein(a) is a surrogate for ascorbate. Proceedings of the National Academy of Sciences of the United States of America, 87(16), 6204–6207. (1990). https://doi.org/10.1073/pnas.87.16.6204
Zelfand E. Vitamin C, Pain and Opioid Use Disorder. Integr Med (Encinitas). 2020 Jun;19(3):18-29. PMID: 33132774; PMCID: PMC7572147.
Boonmark NW, Lawn RM. The lysine-binding function of Lp(a). Clin Genet. 1997 Nov;52(5):355-60. doi: 10.1111/j.1399-0004.1997.tb04353.x. PMID: 9520126.
Björnson E, Adiels M, Taskinen MR, Burgess S, Chapman MJ, Packard CJ, Borén J. Lipoprotein(a) Is Markedly More Atherogenic Than LDL: An Apolipoprotein B-Based Genetic Analysis. J Am Coll Cardiol. 2024 Jan 23;83(3):385-395. doi: 10.1016/j.jacc.2023.10.039. PMID: 38233012; PMCID: PMC7616706.
Long-Term Ascorbic Acid Administration Reverses Endothelial Vasomotor Dysfunction in Patients With Coronary Artery Disease. Noyan Gokce, MD, John F. Keaney, Jr, MD, Balz Frei, PhD, Monika Holbrook, MS, Mariusz Olesiak, BS, Benoy J. Zachariah, MD, Christiaan Leeuwenburgh, PhD, Jay W. Heinecke, MD, and Joseph A. Vita, MD
Norwitz N. Lp(a): The Match, the Fuse, and the Escape Route. StayCurious Metabolism (Substack), Dec 30, 2025. https://staycuriousmetabolism.substack.com/p/the-hidden-mechanism-behind-lpa-riskand