December Newsletter
We’re excited to share a few important updates as we head into 2026—a year of growth, expansion, and deeper commitment to your long-term health.
If we haven’t had the chance to see you recently, McCoy Medical has officially moved into the heart of our quaint Chagrin Falls Village. Our new home at 10 Center Street is now open and fully equipped to support a wide range of preventative and health optimization services. In addition to primary care, we’re offering:
IV therapy (nutritional + therapeutic)
Red light therapy (see the featured article below)
Metabolic testing
Body composition scans
Point-of-care ultrasound
Concierge blood draws
As we approach the new year, many of our patients are updating their lab panels, revisiting their care plans, or scheduling review appointments to set the stage for 2026. If you’re looking to refocus, optimize, or simply check in on your health trajectory, we’d love to support you.
We're also continuing to see patients virtually for those who prefer or need remote care. Whether you're traveling, based outside the area, or simply more comfortable connecting from home, our telehealth services allow us to support both your primary care needs and health optimization journey—no matter where you are.
Let us know how we can help you feel your best heading into the new year.
Don’t worry about sounding professional. Sound like you. There are over 1.5 billion websites out there, but your story is what’s going to separate this one from the rest. If you read the words back and don’t hear your own voice in your head, that’s a good sign you still have more work to do.
Be clear, be confident and don’t overthink it. The beauty of your story is that it’s going to continue to evolve and your site can evolve with it. Your goal should be to make it feel right for right now. Later will take care of itself. It always does.
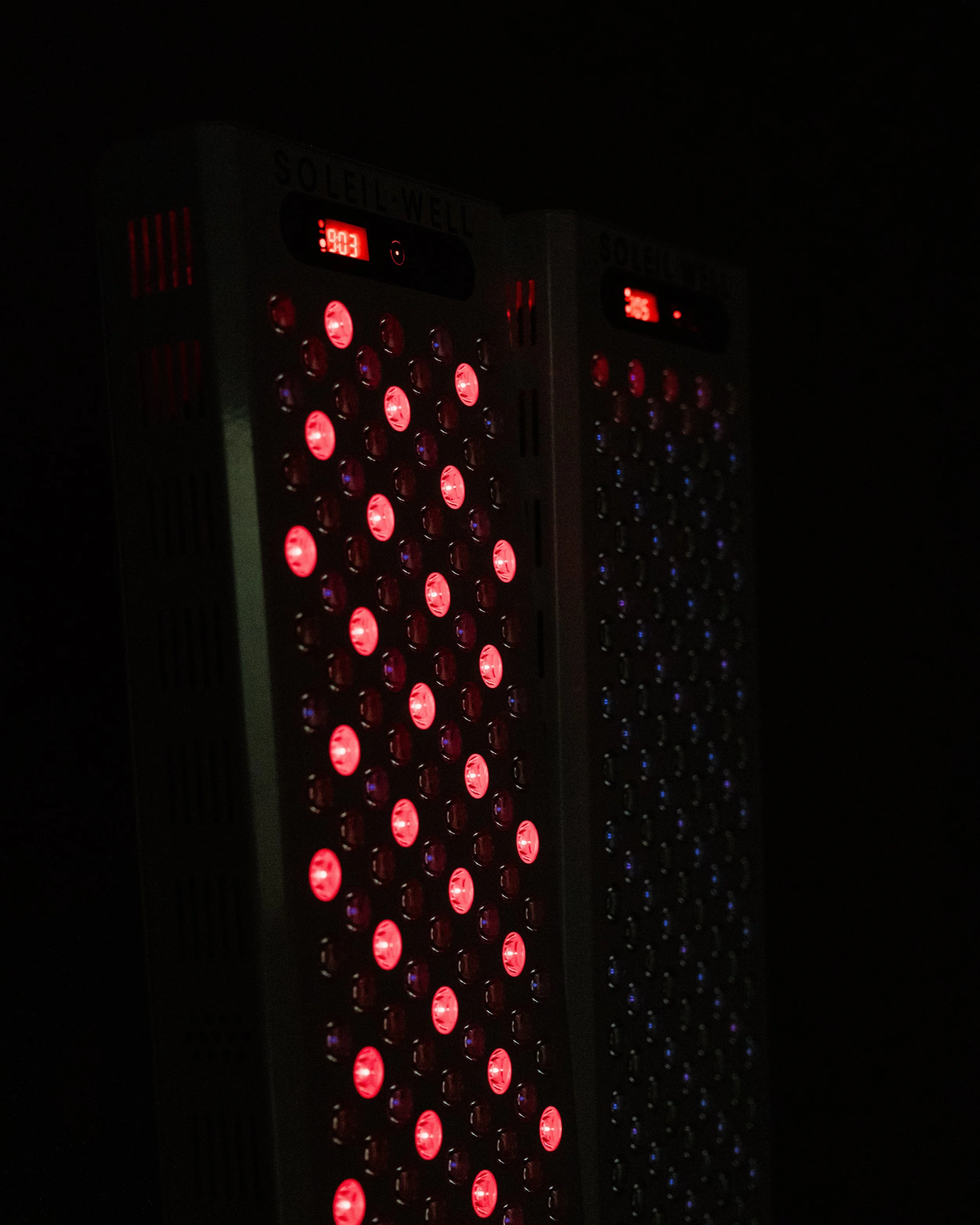
Soleil Well Red Light Panel, available for patient use at the Chagrin Falls Office
Red Light Therapy
Written by Dr. Tom McCoy
If you’ve been with us for a while, you’ve heard me preach the importance of your “light diet” more than once. One of the biggest reasons to get early-morning, full-spectrum light is actually to optimize your sleep that evening. Light exposure shortly after waking helps set your internal circadian clock, drives an appropriate peak in cortisol so it can trend down the rest of the day, and starts the timer on when your melatonin will rise that night.
While morning and evening light strategies get most of the attention, daytime full-spectrum light is also extremely important. Sun exposure has long been associated with decreased all-cause mortality. In one UK Biobank study of more than 376,000 participants, higher sun exposure was linked to a 14% reduction in all-cause mortality, as well as lower rates of cardiovascular disease and even cancer (Stevenson et al., 2023).
So how does that square with what we’ve all been taught about sun, cancer, and DNA damage? As with most exposures, the dose makes the poison. Short, regular doses of full-spectrum sunlight can be very beneficial—as long as we avoid burns. Limiting extended exposure when the UV index is highest (roughly 12–2 pm) is key to reducing that risk.
We can also capture many of the benefits of full-spectrum sunlight by using targeted red and near-infrared (NIR) wavelengths, which have been shown to exert unique, beneficial effects on our biology. Unfortunately, our modern built environments have done an excellent job of eradicating our exposure to natural full-spectrum light, including red and NIR, and that lack likely contributes to higher rates of chronic disease.
One fascinating example: a triple-blind, randomized, sham-controlled trial of red/NIR photobiomodulation (PBM) in ICU patients showed about a 30% decrease in length of stay. This is in critically ill patients (Neto et al., 2024). The potential to reduce cost, complications, and morbidity with a non-invasive therapy is hard to overstate. The study also reported significant improvements in mobility and muscle strength. Given that patients can lose up to roughly 2% of their muscle mass per day in the ICU, anything that mitigates this loss is hugely impactful.
Recently we spent time with our good friends at Continuum Performance in Scottsdale, AZ, where many of our professional athletes train in the off-season. Our MLB guys were there working hard. During that trip, we connected with Kelly Bento, founder of Soleil Well and maker of some of the leading red/NIR clinical therapy devices on the market.
Kelly started Soleil Well out of necessity. A close family member had a major medical event, and after digging into the literature she realized red light could play an important role in his recovery. She was surprised by the lack of quality control and clinical understanding among existing companies, so she started her own. What makes Kelly’s devices unique is her incorporation of specific wavelengths that have demonstrated the most clinical impact. This combination is based on the work of Dr. Tiina Karu, who first identified four key wavelength “windows” that induce photobiological responses. No other company we’ve seen is using this exact approach (Karu, 2013).
After speaking with Kelly, we knew we wanted to bring this therapy to our patients. We were able to secure both a traditional and a custom panel for our clinic at McCoy Medical, and we’re excited to make these available for our members. Below is a brief overview of how photobiomodulation works and where we plan to use it in practice.
What Red/NIR Light Does and How It Works
Energy production
Because of their longer wavelengths, red and NIR light can penetrate deeply—through skin, fascia, muscle, and in some cases even through bone. These photons interact with a mitochondrial enzyme called cytochrome c oxidase, located at complex IV of the electron transport chain. This chain of complexes is responsible for the vast majority of the ATP your body produces every second. When red/NIR light interacts with cytochrome c oxidase, it increases mitochondrial efficiency and can boost ATP production, giving cells more energy to repair, adapt, and function.
Reactive oxygen species (ROS) and inflammation
Excessive ROS is one of the main culprits in accelerated tissue aging and chronic inflammation. PBM appears to act homeostatically—it “reads” the state of the tissue and adjusts ROS accordingly. In healthy tissue, PBM triggers a brief, controlled rise in ROS. That small pulse acts as a signal, kicking off pathways that reduce inflammation overall and improve cellular resilience. In chronically stressed or inflamed tissue, PBM often reduces excessive ROS, helping to restore balance and support healing. In other words, PBM doesn’t just block inflammation; it helps support adaptation by modulating reactive oxygen species in different ways for different tissues.
PBM and immunity
PBM also affects the immune system, especially macrophages—the white blood cells that act as both the seek-and-destroy squad and the cleanup-and-rebuild crew. M1 macrophages are the attack mode, killing pathogens and even cancer cells. M2 macrophages are the heal-and-recover mode, clearing cellular debris, remodeling tissue, and stimulating new blood vessel growth. Red/NIR light has been shown to encourage a shift toward the M2, pro-healing phenotype when that’s what the tissue needs. Similar effects are seen in microglia in the brain, where PBM can help calm neuroinflammation. All of us should be interested in less unnecessary inflammation in the brain.
Practical Applications in the Clinic
Post-operative care and wound healing
There is a substantial body of literature supporting PBM for accelerating wound healing, both in acute post-operative wounds and in chronic, non-healing wounds. By optimizing inflammation—up when needed, down when excessive—and improving mitochondrial energy production, PBM can elegantly support the body’s built-in repair mechanisms. PBM has also been shown to reduce perceived pain, which can improve mobility and recovery after surgery. If you’re facing an upcoming procedure, struggling with a chronic wound, or dealing with ongoing pain, PBM is a powerful adjunct to your recovery protocol.
Arthritis
Both osteoarthritis and rheumatoid arthritis are characterized by elevated inflammatory markers and synovial inflammation. Red/NIR PBM has been shown to lower multiple inflammatory markers and improve pain scores. Used consistently, and ideally earlier in the disease course, it may help slow structural progression while improving daily function (Hamblin, 2017).
Athletic performance and recovery
Multiple studies have shown that PBM can improve exercise performance, increase time to fatigue, and enhance recovery. Red/NIR therapy supports mitochondrial function and local blood flow, which in turn can improve muscle endurance, reduce delayed onset muscle soreness, and speed repair after intense training or competition (Ferraresi et al., 2015). For anyone looking to push performance and recover faster, from weekend warriors to MLB pros, PBM can be a valuable part of the toolkit.
Traumatic brain injury and neurodegenerative disease
Animal models and early human work suggest that PBM can improve cognition and neurological recovery after brain injury. Because energy production, inflammation, and immune activity are all central to neuroinflammation and neurodegenerative processes, PBM may help slow progression and support recovery in select patients when used thoughtfully as part of a broader plan.
Autoimmune conditions
PBM has shown promise in autoimmune models as well. Animal models consistent with multiple sclerosis show improved outcomes with PBM. Human trials in autoimmune thyroiditis (Hashimoto’s) have demonstrated reductions in thyroid antibody levels and decreased requirements for levothyroxine in some patients (Höfling et al., 2013). We’re particularly interested in these applications for patients with autoimmune issues who are already optimizing nutrition, sleep, and stress and are looking for additional, non-drug levers.
At McCoy Medical, we’ll be integrating PBM into post-operative protocols, chronic pain and arthritis treatment, performance and recovery programs, and select neuro and autoimmune cases. If you’re curious whether red/NIR therapy might be appropriate for you, reach out and we can discuss how it could fit into your overall plan.
References
Ferraresi, C., de Sousa, M. V., Huang, Y. Y., Bagnato, V. S., Parizotto, N. A., & Hamblin, M. R. (2015). Time response of increases in ATP and muscle resistance to fatigue after low-level laser (light) therapy (LLLT) in mice. Lasers in Medical Science, 30(4), 1259–1267. https://doi.org/10.1007/s10103-015-1723-8
Hamblin, M. R. (2017). Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophysics, 4(3), 337–361. https://doi.org/10.3934/biophy.2017.3.337
Höfling, D. B., Chavantes, M. C., Juliano, A. G., Cerri, G. G., Knobel, M., Yoshimura, E. M., & Chammas, M. C. (2013). Low-level laser in the treatment of patients with hypothyroidism induced by chronic autoimmune thyroiditis: A randomized, placebo-controlled clinical trial. Lasers in Medical Science, 28(3), 743–753. https://doi.org/10.1007/s10103-012-1129-9
Karu, T. (2013). Is it time to consider photobiomodulation as a drug equivalent? Photomedicine and Laser Surgery, 31(5), 189–191. https://doi.org/10.1089/pho.2013.3510
Neto, R. P. M., Espósito, L. M. B., da Rocha, F. C., Filho, A. A. S., Silva, J. H. G., de Sousa Santos, E. C., Sousa, B. L. S. C., Dos Santos Gonçalves, K. R. R., Garcia-Araujo, A. S., Hamblin, M. R., & Ferraresi, C. (2024). Photobiomodulation therapy (red/NIR LEDs) reduced the length of stay in intensive care unit and improved muscle function: A randomized, triple-blind, and sham-controlled trial. Journal of Biophotonics, 17(5), e202300501.
Stevenson, A., Clemens, T., Pairo-Castineira, E., Webb, D., Weller, R., & Dibben, C. (2023). Higher ultraviolet light exposure is associated with lower mortality: An analysis of data from the UK Biobank cohort study. Health & Place, 89, 103328. https://doi.org/10.1101/2023.07.11.23292360